The plantar fascia is a band of connective tissue that runs along the sole from the heel to the ball of the foot. One of its main roles is to keep the bones and joints in position and enables us to push off from the ground. Bruising or overstretching this ligament can cause inflammation and heel pain. In many cases, plantar fasciitis is associated with a heel spur. Surprisingly, the spur itself does not cause pain, and may often be found in the other foot without symptoms.
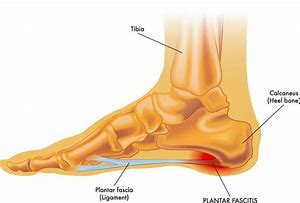
Pain is usually felt on the underside of the heel, and is often most intense with the first steps of the day or after rest. It is commonly associated with long periods of weight bearing or sudden changes in weight bearing or activity.
You may experience:
- Sharp pain in the inside part of the bottom of the heel, which may feel like a knife sticking into the bottom of the foot.
- Heel pain that tends to be worse with the first few steps after awakening, when climbing stairs or when standing on tiptoe.
- Heel pain after long periods of standing or after getting up from a seated position.
- Heel pain after, but not usually during, exercise.
- Mild swelling in the heel.
For most people, the condition improves spontaneously within a year. Treatments that may help control symptoms include:
- Orthotics. A sports medicine professional may prescribe off-the-shelf or custom-fitted arch supports (orthotics) to help distribute pressure to the feet more evenly, and to stimulate the small foot muscles.
- Physiotherapy. A physiotherapist can give instruction on a series of exercises to stretch the plantar fascia and Achilles tendon and to strengthen lower leg muscles, which stabilises the ankle and heel. A physiotherapist may also instruct how to apply athletic taping to support the bottom of the foot.
- Medication, injection and surgery. These measures are for the most persistent cases, and do not replace the need for the treatment methods detailed above.
Aims of rehabilitation
- Decrease initial pain and inflammation.
- Identify biomechanical dysfunction.
- Improve flexibility.
- Strengthen the plantar fascia.
- Return to full fitness.
- Injury prevention.
Return to play
- Follow the advice given by a sports medicine professional.
- After a week of no pain running can be started again.
- This should be a gradual process. If pain is felt at any time then go back a step.
- Running time should be gradually increased.
- Apply tape to the foot to support it for the first few runs, especially if orthotics are not being worn.
- Ensure the correct shoes for your type of running style or sport are worn.
- After every training session apply ice for about 10 minutes.
- Stretch properly before each training session and after. Hold stretches for about 30 seconds and repeat five times.






Leave A Comment